Health News for the
Well-Read Patient
[us_page_title tag=”h2″ align=”center” font=”h1″]
All Articles
Bone Up: What Is Osteoporosis?
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low…
What’s Keeping You Up at Night?
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to…
Pandemic Stress Likely Compounded by Seasonal Affective Disorder
Coping With Sad This Winter As we continue to weather the storm of COVID-19, seasonal affective disorder, or SAD, is once again on our radar. More subtle than an arctic…
New Lung Cancer Screening Recommendations
Spotlighting Both Challenges and Progress This winter the U.S. Preventive Services Task Force (USPSTF) released its new Lung Cancer screening recommendations, lowering both the starting age and pack-year criteria. Previously,…
A Quick Guide to Seasonal Allergies
Pollen, Grass, Ragweed and Mold spores For more than 24 million Americans, the flowering trees and mild weather of spring and summer, signals another allergy season in full bloom. The…
Headaches – Types and Remedies
Oh, My Aching Head A dull pressure, a sharp pain, an uncomfortable pounding, a vise-like sensation – all can signal the start of a headache. A painful part of the…
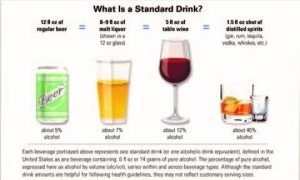
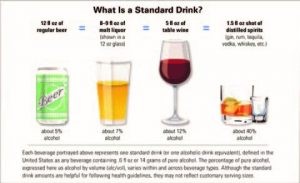
Alcohol: Not Gender-Neutral
The Female Factor: Alcohol is Not Gender-aNeutral Given the growing popularity of the cocktail culture and wine time, it’s important to know that alcohol affects women very differently than men…
Kidney Stones: Treatment & Prevention
This Too Shall Pass: Treating and Preventing Kidney Stones More common, frequently less painful and far more preventable than reputed, kidney stones have, thankfully, entered a new era of highly…
Adult ADD
Attention Please: ADD/ADHD is Not Just a Childhood Condition In the 21stcentury, it’s standard procedure to test unfocused, impulsive and restless children who struggle to achieve in school for Attention…
The Age of Anxiety
Higher Anxiety? Our ‘age of anxiety’ began four centuries ago It can come on suddenly and intensely, causing shaking, confusion and difficulty breathing for no apparent reason…trigger an irrational avoidance…